Abstract
Objective: Hypertension is one of the common risk factors for cardiovascular and cerebrovascular diseases/disorders A developing country like India faces the double burden of communicable and non-communicable diseases; of the which, hypertension is the most important treatable cause of mortality and morbidity with loss of functional capacity and decline in the quality of life.
Aim: To study the prevalence of end organ damage in the hypertensive geriatric age group.
Method: The present study was a cross sectional study, conducted in 150 elderly patients admitted in MGM Hospital, Navi Mumbai, India with the diagnosis of stage I or II hypertension from 2011 to 2013.
Results: Data analysis of the present study showed that 68% of elderly population aged between 60 to 69 years were suffering from hypertension. Compared to males, females had a higher rate of target organ damage. This study found that out of all patients with total end organ damage, 54.6 % had CVS complications, 15.7 % had hypertensive retinopathy, 25.9 % and 18.51 had raised creatinine and proteinuria respectively. 19.4 % had cerebrovascular accident (CVA) complications. Among Cardiovascular related complications Coronary artery disease (CAD) was found in 21 patients, out of them 7 had Congestive cardiac Failure (CCF). Left Ventricular Hypertrophy (LVH) was the most common complication and seen in 38 patients. 13.8 % patients had Regional Wall Motion Abnormality (RWMA)
Conclusion: The present study concluded that Isolated Systolic Hypertension (ISH) is the commonest type of hypertension in geriatric age group. This study concluded that the most common risk factors of HTN in the elderly are sedentary life style, dyslipidemia and extra salt intake while the most common end organ damage was observed to be Left Ventricular Hypertrophy followed by renal dysfunction.
Introduction
High blood pressure is one of the most common risk factors for developing both the cardiovascular and cerebrovascular diseases. During the period of epidemiological transition, developing countries might face the double burden of communicable and non-communicable diseases. Of the non-communicable causes, hypertension is one of the most important treatable causes which is responsible to contribute high f mortality and morbidity around the world. Study found that, systolic blood pressure (SBP) continues to rise until 70-80 years of age while diastolic blood pressure shows the increased trend up to 50-60 years for a normal person [1].
High blood pressure among the elderly age group confers almost three to four fold increase in risk for the development of cardiovascular disease, as compared to the younger. Research suggested that hypertension affects more than half of the people who are aged 65 or older, and the prevalence of hypertension and its related complication continues to rise with age [2].
Hypertension often leads to complications involving the systems like that of cardiovascular, nervous system kidneys, retina etc. Several trials have demonstrated significant rise of blood pressure leading to target organ damage
The aim of the study is to find out the frequency of end organ damage among the hypertensive geriatric patients.
Methods & Materials
The present study was a cross sectional analytic study which was conducted among the 150 elderly patients whose age was above 60 years at MGM Hospital, Kamothe, Navi Mumbai.
Target Organ Damage Definition
End organ damage usually refers to damage occurring in major organs fed by the circulatory system (heart, kidneys, brain, eyes) which can sustain damage due to uncontrolled hypertension, hypotension, or hypovolemia. The present study used the following reference points to conclude the presence of the end organ damage.
For heart: evidence on electrocardiogram screening of the heart muscle thickening up (but may also be seen on chest X-ray) suggesting left ventricular hypertrophy) or by echocardiography of less efficient function (left ventricular failure) [3].
For Kidneys: the presence of leakage of protein into the urine (albuminuria or proteinuria), or reduced renal function [3].
Inclusion & Exclusion Criteria
The participants were selected purposively from 2011 to 2013. Geriatric patients who were hypertensive as per the criteria of Joint National Committee 7 (JNC-7) were included [4]. The patients were later classified according to the target organ complication/s. All other patients below the age of 60 years was excluded.
Data Collection
Clinical evaluation was done by using a structured questionnaire which was prepared following the medical condition. Other information collected was as follows: past or present history of angina pectoris, myocardial infarction, transient ischemic attacks, cerebrovascular disease, hypertensive encephalopathy, renal failure and left ventricular failure based on history or medical records. This was followed by a complete physical examination and necessary investigations like Electrocardiogram, Echocardiographic correlations and end organ complications of cardiovascular, cerebrovascular and renal system. Descriptive statistics were used to present the study findings. The participants were further classified in stage I or stage II as per the JNC-7 criteria. Stage I includes the patients whose blood pressure was between 140-159 mmHg. Stage II included patients having blood pressure above 160 mmHg. All the data management, and data analysis was conducted by IBM SPSS software (Version 20.0).
Ethics
The study proposal was approved by the MGM Medical College’s Ethics Review Committee.
Results
150 elderly patients having stage I or stage II hypertension were studied. 49% patients had systolic blood pressure (SBP) between 140-159 mmHg (Stage I) and 51% patients had SBP > 160 mmHg (Stage II). Out of total patients, 56 (37%) were female and 94 (62%) were male. About 74 patients had stage I HTN while 74 had stage II HTN. Among them 108 (72%) patients developed target organ damage (table 1).
| Category | Frequency | Percentage |
| Gender | ||
| Females | 56 | 37.3 |
| Males | 94 | 62.7 |
| Hypertension Stage | ||
| Stage 1 | 74 | 49.3 |
| Stage 2 | 76 | 50.7 |
| Target organ damage | ||
| Present | 108 | 72.0 |
| Absent | 42 | 28.0 |
| Category | Mean | Standard Deviation (SD) |
| Age (Years) | 67.06 | 6.35 |
| Height (cm) | 161.24 | 11.85 |
| Weight (kg) | 62.58 | 10.15 |
| BMI | 24.36 | 5.04 |
| W/H Ratio | 0.91 | 0.18 |
| SBP | 161.53 | 12.73 |
| DBP | 84.97 | 4.47 |
We found significant correlation between SBP (Stage I and II) and end organ complications. 68% of patients with Stage I Isolated Systolic Hypertension (ISH) suffered target organ damage. 78% of patients with Stage II ISH suffered target organ damage. Hence earlier diagnosis and treatment of ISH would reduce target organ damage. Most common clinical presentation was headache (35%), and dyslipidemia (31%) among the study participants. 24% were smokers and 24% alcoholics and 34% patients were taking extra salt diet. We also found significant correlation (p<0.01) between lipid profile and stage I and stage II HTN (table 3).
| Category | Stage I HTN | Stage II HTN |
| Total Cholesterol | 155 ± 15 | 194 ± 39 |
| Triglycerides | 125 ± 22 | 163 ± 60 |
| High Density Lipoproteins | 54 ± 4 | 39 ± 6 |
| Low Density Lipoproteins | 76 ± 11 | 121 ± 41 |
| Very low density lipoproteins | 25 ± 4 | 32 ±12 |
| p-value | <0.01 | < 0.01 |
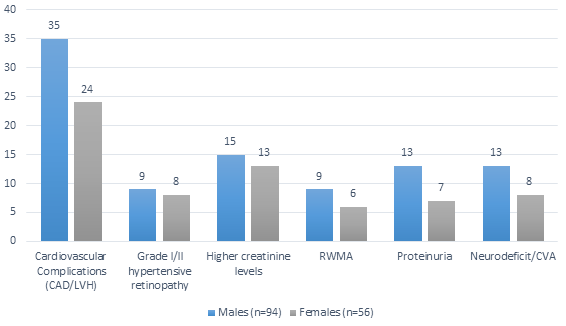
This study found that out of all patients with total end organ damage, 54.6 % had CVS complications, 15.7 % had hypertensive retinopathy, 25.9 % and 18.51 had raised creatinine and proteinuria respectively. 19.4 % had cerebrovascular accident (CVA) complications. Among CVS related complications Coronary artery disease (CAD) was found in 21 patients, out of them 7 had Congestive cardiac Failure (CCF). Left Ventricular Hypertrophy (LVH) was the most common complication and seen in 38 patients. 13.88 % patients had Regional Wall Motion Abnormality (RWMA) (table 4).
| Total end organ damage | Number/108 | Response (%) |
| LVH, CAD | 59 | 54.62 |
| RWMA | 15 | 13.88 |
| Hypertensive Retinopathy | 17 | 15.74 |
| Raised Serum Creatinine (>1.2 mg/dL) | 28 | 25.92 |
| Proteinuria | 20 | 18.51 |
| Neurodeficit/CVA | 21 | 19.44 |
Target organ damage found slightly more in females compared with males (as per percentage) (table 1) & (figure 1).
Discussion
Hypertension is estimated to be the leading cause of current global disease burden and is prevalent in many developing countries, as compared to the developed world. The present literature also suggest the role of low levels of vitamin D, high sugar and fats levels can lead to HTN [5, 6, 7]. Furthermore, it has been proved that HTN could be strongly age dependent which was also observed in Framingham Heart Study [8]. In the present study, there was no significant association between rise in SBP and increase in age. However, there was a positive significant association between end organ complications and increase in SBP and age, thus supporting the results of the previous study [9].
In the present study of 150 patients, there were 94 males and 56 females. Other study found similar male to female ratio, which correlates with our study [10]. In the present study, the most common presentation was headache (35%). We further observed that 13 (8%) patients had a family history of hypertension which other study too had showed as an important determinant of hypertension [11].
In this study only 47 (31%) patients had dyslipidaemia. Another study found dyslipidaemia was present in 55.9% of patients [9]. Due to diagnostic variability there could be different number of patient suffering with dyslipidaemia. Cardiovascular complications (LVH/CAD) in our study was seen in 59 patients. This observation was consistent with one of the previous study [9]. 100 (66%) patients had high SBP as 140 mm Hg and above with normal diastolic blood pressure, out of which 63 (out of those 100 patients {63%}) had at least one target organ damage. The remaining 50 patients had high DBP with normal SBP out of which 39 patients had one or more target organ damage. Oates et al., had found that, more than 40% of the subjects had coronary heart disease, approximately 18% had cerebrovascular disease and almost 10% had chronic renal failure in this study [12].
The previous study reported that high frequency of ISH was present among the elderly hypertensive patients [13]. In one of the studies, 87% patients who developed ISH were in the age of 60 years or above was considered as a category for studying ISH in elderly [9], suggesting age can be an important factor to consider [13, 14, 15].
In our study, CAD was diagnosed in 21 patients out of 108 patients (19.44 %) who developed target organ damage. 12 patients out of those 21, had classical angina supporting other studies which observed 32.3% and 22.82% as an incidence of ischemic heart disease [9, 17]. In our study LVH was found in 38 patients out of 108 target organ damaged patients (35.18 %), while in a study done by Kulkarni et al., [9] observed LVH in 36.8% patients. However, LVH was found in 47% patients in another study [16], while other studies have shown higher LV mass index [15, 18, 19].
In the present study, 15.74 % patients had developed hypertensive retinopathy which was less as compared to another study which also observed hypertensive retinopathy in 50.5% of the total participants [9].
Limitation of the study
The patients were exposed to drugs or medications; which we did not consider in this study. It was a cross sectional and mono-centric study, therefore, longitudinal and multicentre study are expected to find out the risk factor with end organ damage. We also did not identify the date when the patients were diagnosed as hypertensive. The study also did not differentiate between the mono or multi target organ damage.
Conclusion
The presentation of ISH is the commonest type of hypertension in non-obese elderly age group particularly from urban area which may occur due to common risk factors such as hypertension, smoking, non-healthy food intake, sedentary lifestyle, dyslipidemia and extra salt intake. Most common end organ damage in elderly age group is left ventricular hypertrophy followed by renal dysfunction (in the form of proteinuria and raised serum creatinine levels). Target organ involvement increases with age. Hence, care should be taken to maintain the blood pressure levels in order to prevent the complications for the geriatric group.
References
-
WHO Centre for Health Development Ageing and Health Technical Report Volume 5.
A Demographic Analysis - Spectre of ageing population. .
View Article Google Scholar -
Gupta
R,
Kasliwal
RR.
Understanding systolic hypertension in the elderly. The Journal of the Association of Physicians of India.
2004;
52
:
479-85
.
PubMed Google Scholar -
CG34 Hypertension - quick reference guide.
National Institute for Health and Clinical Excellence. 2006.
View Article Google Scholar -
Chobanian
AV,
Bakris
GL,
Black
HR,
et
al.
The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. Jama.
2003;
289
(19)
:
2560-71
.
PubMed View Article Google Scholar -
Mehta
V,
Agarwal
S.
Does Vitamin D Deficiency Lead to Hypertension?. Cureus.
2017;
9
(2)
:
e1038
.
PubMed View Article Google Scholar -
DiNicolantonio
JJ,
Mehta
V,
O’Keefe
JH.
Is salt a culprit or an innocent bystander in hypertension? A hypothesis challenging the ancient paradigm?. The American Journal of Medicine.
2017;
In Press
.
PubMed View Article Google Scholar -
Mehta
V.
Emergence of New Risk Factors for causing Hypertension. Journal of Medical Research and Innovation.
2017;
1
(1)
:
9-11
.
View Article Google Scholar -
Franklin
SS,
Pio
JR,
Wong
ND,
Larson
MG,
Leip
EP,
Vasan
RS,
Levy
D.
Predictors of new-onset diastolic and systolic hypertension. Circulation.
2005;
111
(9)
:
1121-7
.
PubMed View Article Google Scholar -
Kulkarni
V,
Bhagwat
N,
Hakim
A,
Kamath
S,
Soneji
SL.
Hypertension in the elderly. The Journal of the Association of Physicians of India.
2001;
49
(1)
:
873-6
.
View Article PubMed Google Scholar -
Patnaik
BC,
Pandhy
PK.
Hypertension in elderly population. The Journal of the Association of Physicians of India.
1991;
39
(1)
:
160
.
View Article Google Scholar -
Williams
PR.
Will gene markers predict hypertension?. Hypertension.
1989;
14
(6)
:
610-5
.
View Article PubMed Google Scholar -
Oates
DJ,
Berlowitz
DR,
Glickman
ME,
Silliman
RA,
Borzecki
AM.
Blood pressure and survival in the oldest old. Journal of the American Geriatrics Society.
2007;
55
(3)
:
383-8
.
PubMed View Article Google Scholar -
Mahantha
J,
Hazarika
NC.
Hypertension in elderly population of Assam. The Journal of the Association of Physicians of India.
2003;
51
(6)
:
567-73
.
View Article PubMed Google Scholar -
Davis
BR,
Vogt
T,
Frost
PH,
Burlando
A,
Cohen
J,
Wilson
A,
Brass
LM,
Frishman
W,
Price
T,
Stamler
J.
Risk factors for stroke and type of stroke in persons with isolated systolic hypertension. Stroke.
1998;
29
(7)
:
1333-40
.
PubMed View Article Google Scholar -
Heesen
WF,
Beltman
FW,
May
JF,
Smit
AJ,
de
Graeff PA,
Havinga
TK,
Schuurman
FH,
van
der Veur E,
Hamer
JP,
Meyboom-de
Jong B,
Lie
KI.
High prevalence of concentric remodeling in elderly individuals with isolated systolic hypertension from a population survey. Hypertension.
1997;
29
(2)
:
539-43
.
PubMed View Article Google Scholar -
Méndez
GP,
Klock
C,
Nosé
V.
Juxtaglomerular cell tumor of the kidney: case report and differential diagnosis with emphasis on pathologic and cytopathologic features. International journal of surgical pathology.
2011;
19
(1)
:
93-8
.
PubMed View Article Google Scholar -
Krumholz
HM,
Levy
D.
Sex differences in Cardiac adaptation to isolated systolic hypertension. Am J Cardiol.
1993;
72
(3)
:
310-313
.
View Article PubMed Google Scholar -
Jorgensen
HS,
Nakayama
H,
Raaschou
HO,
Olsen
TS.
Effect of blood pressure and diabetes on stroke in progression. Lancet.
1994;
344
(8916)
:
156-159
.
View Article PubMed Google Scholar -
Dickson
ME,
Sigmund
CD.
Genetic basis of hypertension: revisiting angiotensinogen. Hypertension.
2006;
48
(1)
:
14-20
.
PubMed View Article Google Scholar
Comments & Peer Review
Article Details
How to Cite
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Publication history
Accepted: 03-06-2017
Published: 17-06-2017